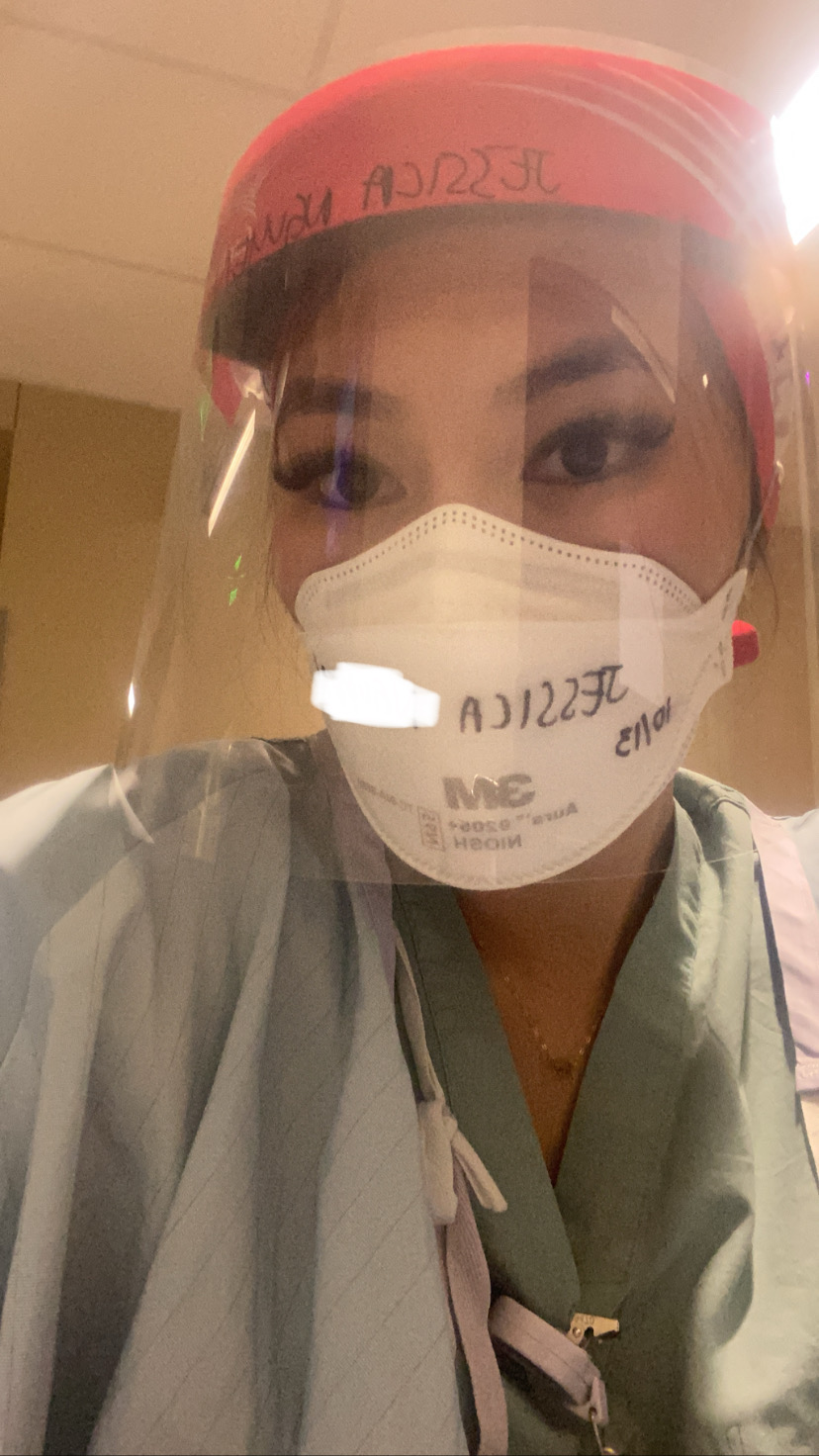
There have been many professions who deal with the ongoing effects of COVID-19, but a lot of my concern goes out to healthcare employees who work on the frontlines. While many roles can easily transition to working from home and dealing with limited complications, nurses must put themselves in harm’s way to take care of those who are critically ill. CDC data, updated on September 27th 2020, shows that over 166,000 healthcare personnel have tested positive for COVID-19. As the nurses continue to play a prominent role in flattening the curve, many deal with their work hours slashed and some are even furloughed. The rippling effects of this even hits nursing students as they see their opportunities for clinical rotations suspended or canceled entirely. But as the media starts to highlight the heroic stories within the emergency room, it brings up the question if this pandemic can create positive changes for those interested in nursing. Between the new opportunities in telehealth and increased flexibility to work in different departments, nurses could still find ways to be reinvigorated in their work. I reached out to Jessica, an ICU nurse in the DFW area, to discuss how nurses have been adapting to COVID-19. She has stated that these are her opinions and not representative of her company.
Hello Jess, the American Nurses Association conducted an April 2020 survey of 32,000 nurses and found that only 11% believed they were well-prepared to care for patients with COVID-19. What skills and education have you or other nurses needed to be prepared for COVID-19 situations and will this pandemic highlight the need for any specific training?
Covid-19 patients are the sickest patients in the hospital and quickly decompensate due to respiratory failure and require ventilator support. We work tirelessly alongside our doctors and respiratory therapist working 13 hour shifts in our PPE the whole time. Covid not only affects the lungs but many other organs as well, causing MODs multiple organ dysfunction syndrome. Many covid patients’ kidneys go into “shock” and need to be on CRRT, continuous renal replacement therapy is a type of dialysis that functions as an external kidney to filter their blood and regulate electrolytes. Managing the CRRT machine has been a new skill I have learned due to so many patients requiring CRRT. Another skill I have acquired is precepting new nurses during the surge in positive cases we experienced this summer. FEMA, the natural disaster organization provided financial support to hire ICU nurses from all over the states to help my hospital back in August. I was fast tracked into training new nurses who came from smaller hospitals that didn’t have experience in high acuity cases. Most Covid patients were maxed out on almost all their infusions such as their sedation, paralytics, and vasopressors that help raise their blood pressure. I definitely learned time management, I was constantly running back and forth replacing these infusion bags while helping manage their ventilator and CRRT dialysis machine, titrating these vasopressors to make sure the patients’ blood pressure wouldn’t tank, on top of training a “new” nurse. We are in dire need of ICU nurses with strong critical thinking with experience in ventilator management, CRRT, and other life sustaining equipment.
There’s a saying by some healthcare administrators that “a nurse is a nurse is a nurse”. A June 2020 report by the American Hospital Association estimated that U.S hospitals will lose 323 billion dollars this year due to COVID-19 effects, which will be followed with more layoffs and healthcare systems will possibly set higher expectations from the remaining nurse staff. Could this pandemic create situations where specialized nurses in the OR, ER, ICU, or medical-surgical floor are expected to help out in completely different departments?
From my experience, when COVID-19 hit, the ICU was at max-capacity and hit a surge during summer months. At a high point, we had over 200 patients coming into the department and had to figure where to put everyone. During this volatile time, state restrictions had elective surgeries put on hold and only emergency operations were allowed. These state and national regulations have had a clear effect on clinics, operating rooms, and other medical departments. The nurses from these effected departments were still able to really help the ICU in the setup of personal protective equipment and restocking inventory. Med/Surg nurses, the largest nursing specialty, have also contributed to the ICU during COVID-19 like helping turn over our patients or assisting in the bathing schedule. While they take care of non-emergent situations, we can focus more on the management of critical systems. It doesn’t surprise me that the med/surg nurses could assist in these responsibilities, because they’re used to strict time-management and handling 5 patients at a time. This pandemic has also highlighted the importance of the fellowship programs offered in different healthcare systems, so that a nurse can transition effectively into a new field if their department is experiencing layoffs.
You have stories like Angela Ramos, a second-year nursing student at Indian River State College, who is now doing virtual simulations instead of a clinical rotation. Do you think there will be a rocky transition to overcome for the newest round of nursing graduates with possibly less in-person department experience?
Any graduate who is learning from a virtual simulator instead of physically attending a clinical rotation will have a rocky transition. What you learn in nursing school will not fully cover everything that can pop up in real life scenarios. Outside of clinical rotations, there are various residency programs offered that can help stress the importance of different medications and show you different conditions in-person. I’m actually precepting for a new student who got accepted into a 5 month residency program and will help them navigate some of the new dilemmas that appear during this pandemic. I would avoid sending new grads right to the front lines of the ICU, because that’s a scary situation that a student shouldn’t be dealing with early in a residency program. That also can be a misuse of limited personal protective equipment during a time of vulnerable supply lines. It’s important to find that balance between presenting realistic scenarios within the residency programs offered but also creating an environment where the student can succeed.
Amanda-Jane Weir, the NHS Foundation’s head of staff engagement, said patients being cared for by healthcare staff in PPE could feel isolated. Is there a way that nurses can maintain human connection with patients in a landscape of social distancing, visitor restrictions, and PPE attire?
I’ve met various travel nurses who have told me about their experiences getting sick at work. They expressed that it was a discomforting period where staff members didn’t want to talk to them and even tried to limit the amount of times they were in the same room as the infected nurse. I’ve also heard stories from patients who have stated they didn’t even know what their nurse looked like, which can obviously be a negative experience if they’re spending weeks being taken care of. Some hospitals have made solutions like having nurses print photos of themselves to attach to their gowns, which makes the experience more personal for both parties involved. Our department has allowed zoom calls during this pandemic so patients can speak with their families and have recently allowed in-person visitation. We have to be careful though, so we place age-restrictions on these visits and make sure we limit the visit to one person at a time.
Black people represent 6% of Wisconsin’s population, but account for almost half of the state’s coronavirus deaths. Black people also account for two-thirds of Chicago’s deaths despite being less than one-third of its population. Do you think this staggeringly disproportionate reality will create a long-overdue response by the government, public, and/or other organizations in addressing racial disparities?
I have noticed a large percentage of the patients effected are African-American and Hispanic, but I’m not sure if this points to a specific reason. These groups could possibly be in more compact living situations, dealing with tightly-knit communities, or attending more in-person gatherings. With that being said, I wouldn’t want anyone to think their demographic is exempted from the dangers of getting sick due to this pandemic. For example, you’ve had many people state that children couldn’t get infected because of the low cases reported on young age groups. In reality, this might be occurring because children are at home more often and won’t be hit by the first wave of infections.

